Unlocking the Secrets of a Blood Parasite

It’s an unnerving thought: tiny worms burrowing into your skin, living in your veins and arteries, wreaking havoc on your body from the inside out.
But it’s reality for the millions around the world who suffer from schistosomiasis, a disease caused by a genus of parasitic worms called Schistosoma. Depending on the species, these small invaders can cause abdominal pain, diarrhea, organ damage, and worse. Schistosomiasis is estimated to kill over 11,000 people globally every year, according to the World Health Organization (WHO).
Kate Rawlinson, an assistant scientist in the Josephine Bay Paul Center at the Marine Biological Laboratory (MBL), researches Schistosoma mansoni, which causes schistosomiasis in the intestines. Many scientists at the MBL study novel research organisms in hopes of answering broad biological questions, but Rawlinson’s work on S. mansoni is different.
“We’re studying it for its own self because it is a major pathogen,” she said. “By studying it at the cell and molecular levels, we can understand how it develops, how it infects its host, and which genes are expressed where, in order to look for new vaccine and drug candidates to try and control the parasite.”
Rawlinson is tackling these questions alongside Teresa Attenborough, a bioinformatician at the University of Glasgow. Attenborough recently completed a Whitman Center Fellowship at the MBL, embedded in Rawlinson’s lab. The pair used the time to jumpstart a catalog of the roughly 1,500 cells that make up one of S. mansoni’s larval stages, called the cercariae.
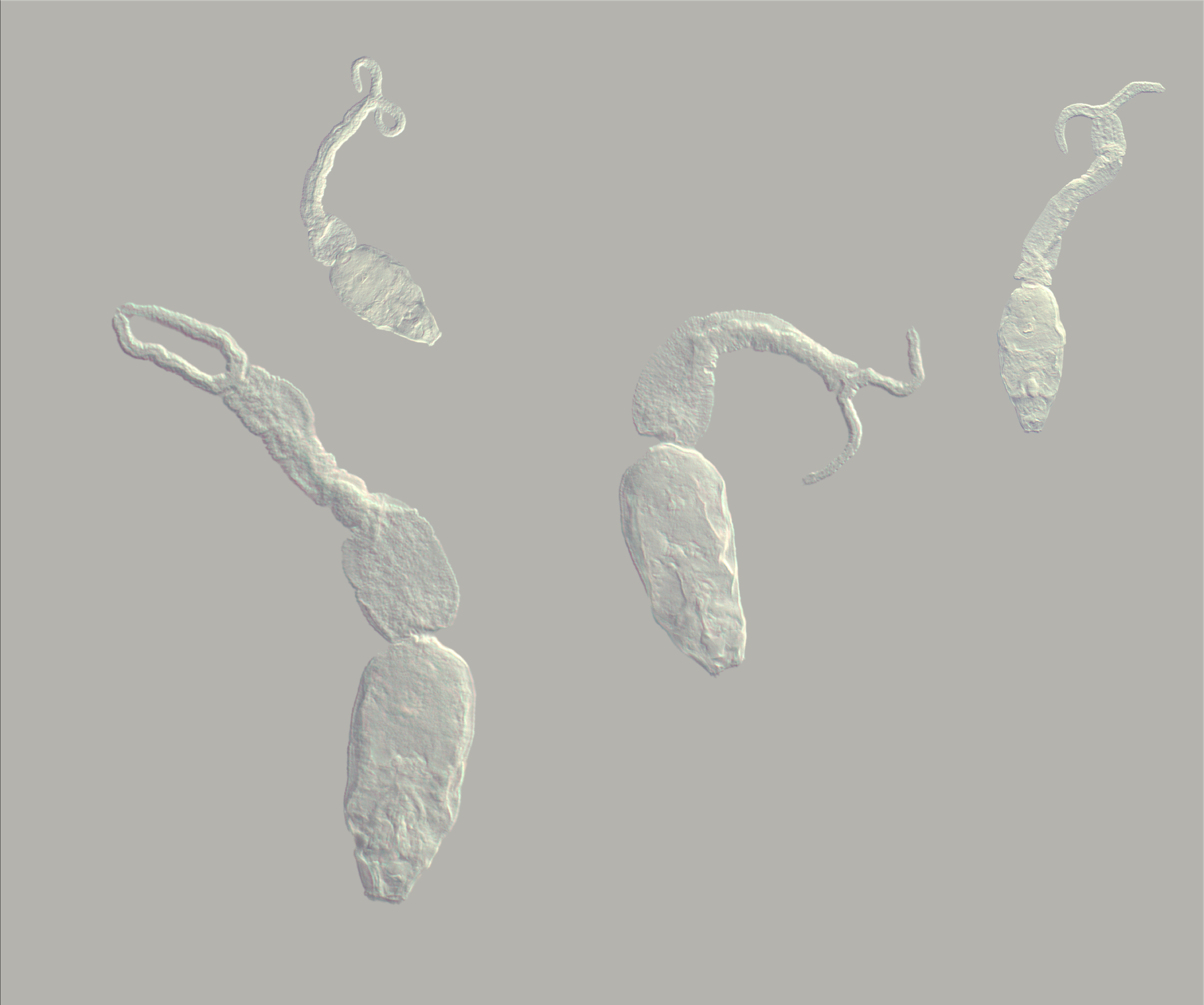
S. mansoni changes form several times throughout its life; cercariae is the stage at which the worm infects humans. The total number and function of the cells at this stage is unknown, Attenborough said.
“So we're trying to understand more about that, and we're hoping in the long-term to put together all these different snapshots at different life stages,” she said. “Again, if we're thinking about a vaccine, what kind of genes and gene products can you target at different stages that are still present as the worm changes?”
A disease of global significance
S. mansoni spends most of its life inside either a snail host or a mammalian one and has two short-lived larval stages, where it lives in freshwater. Inside a human host, adults roughly a centimeter long survive in the blood vessels lining the intestines, laying hundreds of eggs per day—sometimes for up to a decade or more.
About half of these eggs are excreted in feces, Rawlinson said, but the other half get lodged in tissues and organs such as the liver. The human immune system reacts defensively, encapsulating the foreign eggs inside structures called granulomas.
“And the more eggs, the more encapsulated structures are found in our liver, which makes the organ hard,” Rawlinson said. “And it means that our liver function goes down. We've got this really hard liver that's not functioning properly, and that's what causes a lot of the pathology in the disease.”
WHO recommends praziquantel for prevention and treatment of the disease; though the drug is safe, effective, and low-cost, it has limited availability, the organization says.
Combining years lost to premature death and years lived with a disability, schistosomiasis is responsible for 2.6 million years of lost health, Rawlinson’s lab website says. In 2021, WHO adopted a road map on neglected tropical diseases that set out to eliminate schistosomiasis as a public health problem in endemic countries by 2030.
“It's a really nasty parasite,” Rawlinson said. “An important parasite.”
Building a cell atlas
To build the cell catalog, or atlas, Rawlinson and Attenborough first harvest cercariae from infected snails. They collect and isolate individual cells from the cercariae and use a technique called single-cell RNA sequencing to determine which genes are being expressed—or switched on—in specific cells.
Attenborough then uses software programs to group the cells together based on the similarity of their gene expression. If a specific gene is only switched on in certain cells, those cells are likely the same type.
Once they’ve found genes characteristic of certain cell types, Rawlinson and Attenborough use an imaging technique called in situ hybridization to visualize where those genes are being expressed in cercariae—and as such, where those cell types are located within the worm.
“We're at the stage now where we can look at this multicellular parasite at a resolution that has never been looked at before,” Rawlinson said. “We can dissociate the cercariae into a soup of its own cells, sequence the RNA from each cell, group these cells computationally based on their gene expression, identify genes that represent each cell type and look at where they are expressed in the animal. This gives us information about the cell and tissue architecture of the larva and also helps us understand the function of different cell types, for example, whether a neuron might be sensory or motor.”

A powerful partnership
As Rawlinson and Attenborough fill out their cercariae atlas, they can compare their findings to other S. mansoni stages, learning more about how the dangerous parasite develops through its life cycle.
The pair’s first project together was a cell atlas for S. mansoni’s first larval stage, miracidium. That was in the United Kingdom. Rawlinson later moved to the United States, but the MBL’s Whitman Center Fellowships—which allow visiting scientists to conduct research at the MBL for four to 10 weeks—gave the duo the chance to reunite in person.
Their different skill sets—Rawlinson an expert in the lab, Attenborough in computational biology—are natural complements. Seeing their work from both the wet and dry lab angles gave both a greater understanding of the whole project, Rawlinson said.
Attenborough’s fellowship wrapped up in June, but she and Rawlinson are continuing to collaborate remotely on the cercariae atlas.
“I couldn't do this without Tess,” Rawlinson said.
“And I couldn’t do this without Kate,” Attenborough added.